Pre-Exposure Prophylaxis (PrEP): A Key Pillar In Ending the HIV Epidemic
By Dr. Iheanyichukwu Samuel Onwubiko
The “Ending the HIV Epidemic Initiative: A Plan for America” (EHE) is a federal effort to reduce new HIV infections in the United States by 75% in five years and by 90% in ten years and includes four “pillars”:
- Diagnose
- Treat
- Prevent
- Respond
It is a 10-year plan with two phases:
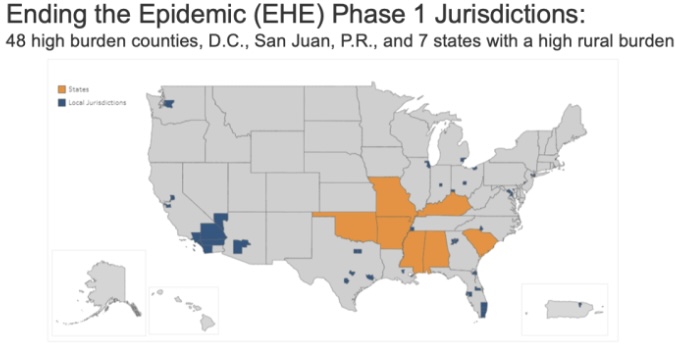
- Phase I: From 2020 to 2025 focuses efforts on the regions hardest hit by the HIV epidemic (48 counties, 7 states). More than 50% of HIV diagnoses in the US occur in these 48 counties, D.C., and San Juan
- Phase II: From Year 2026 to 2030 within which efforts will be more widely disseminated across the nation.
- Phase III will focus on providing care and treatment and intensive case management aimed at keeping the number of new HIV infections below 3,000 per year
How committed is the US Government to Ending the HIV Epidemic (EHE)?
The commitment to “ending the HIV epidemic” has been accompanied by additional federal funding to the amount of $1.75B just for the first phase. The breakdown is as follows:
- FY2019 – Congress reprogrammed funding from other sources amounting to $34.68m.
- FY 2020 – Congress appropriated $267m
- FY 2021 – Congress appropriated $404.75m.
- FY 2022 – Congress appropriated $473.25m
- FY 2023 – Congress appropriated $573.25m.
In 2019, a spark ignited the Ending the HIV Epidemic (EHE) initiative with $35 million reallocated from the Secretary’s Minority AIDS Initiative Fund. That spark has grown into a wildfire of commitment, with annual funding steadily increasing to $573.25 million in 2023. This financial firepower isn’t just about numbers; it’s an evidence of the dedication to tackling this critical public health challenge head-on.
To make a real impact, these funds have been strategically distributed across the frontlines of the EHE battle. From direct patient care, ensuring those living with HIV have access to the support they need, to groundbreaking research that paves the way for new prevention and treatment options, every dollar is working towards a future free from HIV.

PILLARS OF THE INITIATIVE
There are four “pillars” to the initiative that serve as a road map for achieving EHE goals:
Diagnose: Currently, 14% of people in the United States with HIV are unaware of their infection and 40% of all new HIV infections result from someone who did not know they were HIV positive. This strategy pillar seeks to diagnose all people in the US as soon as possible after infection.
Treat: HIV Treatment is important for optimal individual health outcomes and harnessing the benefits of “treatment as prevention”– that is when someone is virally suppressed, they cannot transmit HIV to others. This pillar aims to treat people with HIV rapidly after diagnosis to help achieve and maintain viral suppression.
Prevent – While the rate of new HIV infections has slowed since its peak, progress has stagnated in recent years and racial disparities persist. The prevent pillar seeks to use proven prevention interventions to stop new HIV infections from occurring with a specific focus on bolstering PrEP uptake.
Respond – The respond pillar is focused on rapidly responding to potential HIV outbreaks to disseminate prevention and treatment services as needed and in part relies on harnessing public health strategies, such as molecular surveillance.
PrEP: YOUR PROTECTION AGAINST HIV
What is PrEP?
PrEP, or Pre-Exposure Prophylaxis, is a daily medication that can significantly reduce your risk of getting HIV from sex or injection drug use. It’s a safe and effective way to protect yourself, especially if you’re at higher risk for HIV infection.
Importance of PrEP in the US
- Pre-exposure prophylaxis (PrEP) is a highly effective medication for preventing HIV infection. It plays a crucial role in the fight against the HIV epidemic in the United States, particularly in areas with high rates of new HIV diagnoses, such as Baltimore.
Effectiveness of PrEP
- Efficacy: PrEP reduces the risk of getting HIV from sexual contact by about 99% when taken as prescribed and by at least 74% among people who inject drugs.
- Prevention: PrEP is a key tool in preventing HIV transmission, especially in high-risk populations, including men who have sex with men (MSM), transgender individuals, and people who inject drugs.
Current HIV Burden in the US
- Prevalence: Approximately 1.2 million people in the United States are living with HIV.
- New Diagnoses: There are nearly 37,000 new HIV diagnoses each year in the US.
- Geographic Focus: The Ending the HIV Epidemic (EHE) initiative targets 48 counties, Washington D.C., San Juan, Puerto Rico, and seven states with substantial rural HIV burdens, which account for more than 50% of new HIV diagnoses.
PrEP Uptake and Disparities
- Low Uptake: Despite its effectiveness, less than 25% of people in the US who could benefit from PrEP were taking it as of 2019.
- Racial Disparities: Significant inequities exist in PrEP use among different racial and ethnic groups. For example, in 2021, there were only 3 Black and 6 Hispanic/Latinx PrEP users for each new HIV diagnosis within those groups, compared to 26 white PrEP users for each new HIV diagnosis among white people.
- Regional Disparities: The Southern US, which accounted for 52% of HIV diagnoses, had only 39% of PrEP users
These figures suggest that Black residents face more barriers in progressing through the PrEP care continuum from screening to prescription. Addressing these disparities is crucial for equitable HIV prevention.
Who should consider PrEP?
You might want to consider PrEP if you:
- Are sexually active and don’t always use condoms
- Have a sexual partner who has HIV
- Have been diagnosed with a sexually transmitted infection (STI) in the past 6 months
- Inject drugs
How does PrEP work?
PrEP contains two medications that work together to prevent HIV from establishing an infection in your body. When taken daily, it can reduce the risk of getting HIV from sex by about 99% and from injection drug use by at least 74%.
Approved Medications:
- Truvada (Tenofovir Disoproxil TDF/Emtricitabine FTC)
- Descovy (Tenofovir Alafenamide TAF/FTC)
- Apretude (cabotegravir injectable)
Is PrEP covered by insurance?
Most health insurance plans cover PrEP, including Medicaid and Medicare. If you don’t have insurance, there are programs that can help you access PrEP at a reduced cost or for free.
Remember:
- PrEP is not a substitute for condoms, which also protect against other STIs.
- You need to take PrEP daily for it to be most effective.
- Talk to your doctor or a healthcare provider to learn more about PrEP and whether it’s right for you.
The FUTURE of PrEP (Lenacapavir)
Lenacapavir (Sunlenca), the groundbreaking medication currently used for multidrug-resistant HIV treatment, is showing immense promise in clinical trials for PrEP (pre-exposure prophylaxis). If successful, this could revolutionize HIV prevention, as Lenacapavir’s long-acting nature means PrEP users might only need two injections per year. This would not only be more convenient but also potentially improve adherence and accessibility, offering a new level of protection against HIV acquisition. Stay tuned for updates on this groundbreaking research!
Together, we can end the HIV epidemic and PrEP is a powerful tool that can help us get there.